Unlocking the Mystery of Chronic Pain: A New Brain Pathway Identified
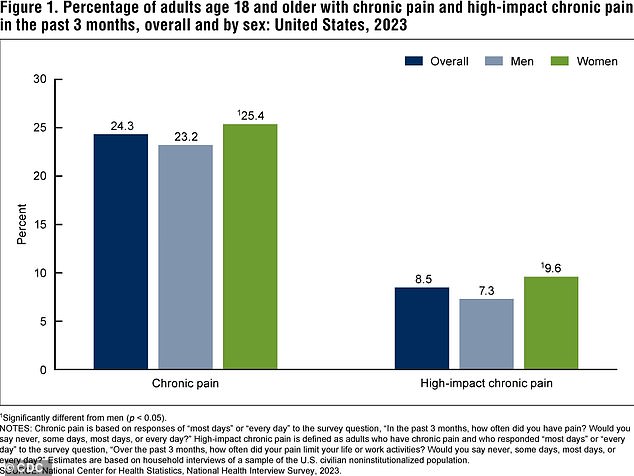
For a significant portion of the population, chronic pain is a relentless adversary, dictating the rhythm of daily life and often necessitating a complex regimen of medications. In the United States alone, an estimated one in five adults grapples with this persistent affliction, with recent surveys highlighting that three out of every four individuals experiencing chronic pain also face some degree of disability. This can severely impede their ability to work, engage in daily activities, and maintain a good quality of life.
The origins of chronic pain, whether it manifests in the shoulders, back, knees, or feet, have long been a subject of intense scientific debate, with no definitive answers emerging. However, a groundbreaking study from researchers at the University of Colorado Boulder may have just uncovered a crucial clue, shedding new light on how temporary discomfort can evolve into long-lasting suffering.
Pinpointing the Brain's Chronic Pain Circuit
The research team focused their efforts on understanding the intricate transition from acute, short-term pain to chronic, persistent pain. Their investigation zeroed in on a specific neural pathway connecting two key areas of the brain: the caudal granular insular cortex (CGIC) and the primary somatosensory cortex.
- Caudal Granular Insular Cortex (CGIC): This is described as a small cluster of cells, roughly the size of a sugar cube, situated deep within the insula, a brain region responsible for processing bodily sensations.
- Primary Somatosensory Cortex: This area is crucial for perceiving physical sensations such as pain and touch.
To explore this pathway, the researchers utilised mouse models engineered to mimic chronic pain conditions, particularly those affecting the sciatic nerve. The sciatic nerve, the longest and largest nerve in the body, extends from the lower spine all the way down to the feet. Injuries to this nerve are known to cause allodynia, a condition where normally non-painful stimuli, like light touch, are perceived as intensely painful.

The CGIC's Pivotal Role in Sustaining Pain
Through the strategic use of gene editing to deactivate specific neurons, the study revealed a fascinating dynamic. While the CGIC appeared to play a relatively minor role in the processing of acute pain, it was found to be instrumental in sending signals to brain regions responsible for pain processing. These signals effectively instructed the spinal cord to maintain the state of chronic pain, preventing it from subsiding naturally.
Conversely, when the researchers inhibited the activity within this CGIC pathway, a significant reduction in pain was observed in the mice. Crucially, this intervention also successfully halted the development of allodynia, suggesting that this specific brain circuit is a key player in the perpetuation of chronic pain.
Implications for Future Treatments
Professor Linda Watkins, a senior author on the study and a distinguished professor of behavioral neurosciences at the University of Colorado Boulder, elaborated on the significance of their findings. "Our paper employed a variety of state-of-the-art methods to define the specific brain circuit that is crucial for the decision-making process of pain becoming chronic and for instructing the spinal cord to carry out this command," she stated. "If this critical decision-maker is silenced, chronic pain does not occur. If it is already ongoing, chronic pain melts away."
The most prevalent forms of chronic pain in the United States include back pain, headaches and migraines, and joint conditions like arthritis. These conditions collectively account for nearly 37 million doctor's appointments annually. Worryingly, approximately one in three American adults experiencing chronic pain report a lack of a clear diagnosis or an identifiable reason for their suffering.
The Sciatic Nerve Study in Detail
The research, recently published in The Journal of Neuroscience, involved inducing injuries to the sciatic nerves of mice. Pain in this region, known as sciatica, affects an estimated 3 million Americans. The researchers meticulously measured the sensitivity of the mice's paws to touch and analysed brain and spinal cord activity to assess their pain levels.
Their findings indicated that the CGIC transmits widespread signals to the primary somatosensory cortex, a region located in the brain's parietal lobe that handles sensory input like touch, temperature, pain, and pressure. Activation of the CGIC was directly linked to the manifestation of chronic pain.
Jayson Ball, the lead author of the study and a scientist at the brain health startup Neuralink, explained the mechanism: "We found that activating this pathway excites the part of the spinal cord that relays touch and pain to the brain, causing touch to now be perceived as pain as well."
Gene Editing Offers Hope for Pain Relief
The research team then employed gene editing techniques to suppress the activity of the CGIC. This intervention led to a measurable decrease in brain and spinal cord activity, even in mice that had been experiencing pain for several weeks – a duration considered equivalent to years in human terms.
Ball emphasised the study's contribution to the broader understanding of chronic pain. "This study adds an important leaf to the tree of knowledge about chronic pain," he remarked. "Our research presents a clear case that specific brain pathways can be directly targeted to modulate sensory pain."
The Path Forward: Human Trials and New Therapies
While these findings are highly promising, the researchers acknowledge the need for further studies to fully elucidate the relationship between the CGIC and chronic pain, particularly in human subjects. "Why, and how, pain fails to resolve, leaving you in chronic pain, is a major question that is still in search of answers," Professor Watkins noted.
Despite this, Ball expressed optimism about the potential for translating these discoveries into tangible treatments. "Now that we have access to tools that allow you to manipulate the brain, not based just on a general region but on specific sub-populations of cells, the quest for new treatments is moving much faster," he concluded. The identification of this critical brain circuit opens exciting avenues for the development of novel medications and therapeutic interventions aimed at alleviating the burden of chronic pain for millions worldwide.


No comments:
Post a Comment